The Long Road

Mia Carter was on vacation in Colorado’s San Juan Mountains when she started to feel like she was dying. It was late in the summer of 2020 and for months, Carter had been grappling with the lingering effects of a COVID infection she had contracted when the first viral wave swept across the U.S. As the virus worked its way through her body, Carter rapidly lost the ability
to breathe and was whisked off to Austin’s overwhelmed St. David’s Medical Center, where she was treated for bronchitis and asthma. After a few hours in the hospital, Carter was discharged with a prescription for prednisone—a steroid typically used to treat inflammation—and instructions to take it easy at home until she recovered. But that recovery never came.
Over the next six months, Carter attempted to carry on with her life as it was before. She had hardly missed a day of work as a professor of English and associate dean of Student Affairs at UT, despite constantly feeling exhausted and experiencing a painful feeling of constriction in her chest. Before COVID, Carter was a competitive rower and avid swimmer, but now it was hard for her to muster the energy to even leave the house.
“I just kept battering on because a lot of people depend on me, but I never felt like I was getting better,” Carter says. “People would look at me and say, ‘Oh, you look great,’ but they couldn’t see what was going on in my body or know how difficult it is to go from being super athletic to feeling like I’m going to die earlier than I thought I would.”
In August of 2020, on a getaway with her husband in Colorado, Carter started to feel as if she were having a stroke. It was the first of many stroke-like episodes over the next several weeks. She checked into the hospital each time, but when her tests came back normal, the doctors would send her home with instructions to rest. On the fourth time this happened, Carter checked herself into a cardiac clinic. It was only then that doctors were able to pinpoint what was going wrong: Carter had blood clots throughout her lungs and another blood clot in her left arm. She was immediately hospitalized and put on a blood thinner, but her health continued to deteriorate. She developed gastrointestinal issues, severe insomnia, and her breathing issues intensified. “I thought the stroke was going to be the most dramatic part of all this, but things just kept getting worse,” Carter says.
She was starting to lose hope that she would ever recover. Then one day, her endocrinologist referred her to Esther Melamed, a neurologist and assistant professor in the Department of Neurology at Dell Medical School. Melamed was helping to lead a new “Post-COVID-19” program at UT Health Austin—the clinical practice of Dell Medical School—that was designed to study and treat people suffering from the long-term effects of COVID infections. Although Carter didn’t know it at the time, it was an introduction that would finally put her on the road to recovery.

The Mystery of Long Covid
Current estimates suggest that around half of all American adults have been infected with COVID-19 at some point in the past three years. While most people infected with COVID make a full recovery, a subset of patients will continue to have complications from the illness for months—often years—after the initial infection. It’s unknown exactly how many people have experienced “long COVID,” but the U.S. Centers for Disease Control says it likely impacts about one out of every five adults who have contracted the virus.
Getting a solid estimate on how many people have long COVID is tricky because the symptoms are highly variable and there is no way to test for it. Some of the most common symptoms associated with long COVID are a loss of taste and smell, trouble concentrating, shortness of breath, and lingering fatigue. Like Carter, many people also experience an elevated heart rate, dizziness, and chest pain. Some have even reported losing teeth, a sense that their body is vibrating, and a bacterial infection called “black hairy tongue.”
The challenge for doctors is that these symptoms persist long after the person stops testing positive for COVID, and tests for other illnesses typically come back negative. From the doctor’s perspective, the patient appears perfectly healthy even though they are reporting a significant amount of physical pain and psychological distress. But the staggering variety of symptoms means that doctors can’t even agree on a definition of long COVID, much less get to the root of its causes and treatments.
UT Health Austin’s Post-COVID-19 Program was designed to change that. In late 2020, after it was apparent that many people were suffering from lingering symptoms after a COVID infection, a small group of UT researchers and clinicians banded together to build a specialized program that would both research the causes of long COVID while providing specialized care for members of the local community.
“We decided that we couldn’t wait for the book to be written about long COVID,” says Michael Brode, an assistant professor in the Department of Internal Medicine at Dell Medical School and the medical director of UT Health Austin’s Post-COVID-19 Program. “We just needed to start seeing patients and figuring it out as we went.”
UT Health Austin’s program was originally conceived as a transition clinic for COVID patients whose symptoms were severe enough to place them in an intensive care unit at the hospital, but Brode says that those have turned out to be the minority of the roughly 400 patients the program has seen to date. Instead, most of the patients seen at UT Health Austin haven’t been hospitalized for their COVID infections, but are dealing with ongoing symptoms that lack any other explanation. “The people we’re seeing have this mysterious illness and didn’t know where else to turn,” Brode says.
The program is designed to help patients cope with the realities of their chronic illness and give them the best possible shot at recovery. When a patient first enters the program, says Brode, most of the initial treatment is helping them effectively manage their energy. As Carter found out firsthand, the natural reaction to long COVID is to try to power through it as if nothing was wrong. But ignoring the fatigue can make recovery more difficult, so Brode helps patients adjust their expectations around what they can manage day-to-day. “I think it makes people feel better when we have a heart-to-heart about what they’re going through and they recognize that other people feel the same way,” Brode says.
Another important step in the Post-COVID-19 Program is symptom management. Although there is no known cure for long COVID itself, Brode and his colleagues can offer patients medications that will address their unique symptoms. Carter, for example, was put on a regimen of Intravenous Immunoglobulin (IVIG) therapy, which is typically used to treat immune system disorders. This isn’t a treatment that would work for every patient that comes through the clinic, and it is still considered an experimental treatment for COVID. But because the program’s clinicians can work closely with their patients and researchers at UT, they are able to identify tailored therapies that physicians who don’t specialize in long COVID might miss. “We have a pretty in-depth conversation with patients about where the research is on experimental medications and what the risks versus benefits are,” Brode says.
Of course, the effects of long COVID aren’t purely physical. Like other patients with chronic diseases, people suffering from long COVID must also grapple with the psychological distress of having their lives turned upside down. Anxiety and depression in long COVID patients are common. For patients like Carter, it might arise from no longer having the energy to do physical activities they once loved, fears about dying, and frustrations with not being able to accomplish simple daily tasks. To help these patients, UT Health Austin’s Post-COVID-19 program provides patients with individual therapy and strategies for self-care.
Aaron Braverman is a clinical social worker in the program and a member of UT Health Austin’s Integrated Behavioral Health team. Braverman is an expert in helping people learn how to cope with the mental distress that often accompanies severely disabling illnesses and has adapted many of these techniques to help patients with long COVID. For example, one of the most common techniques Braverman uses is called acceptance and commitment therapy, which is fundamentally about accepting things that are beyond a person’s control and committing to actions that can enrich their life.
“There are multiple kinds of psychotherapy that can be applied to patients with long COVID, and there’s no evidence that we should use one modality instead of another for treatment,” Braverman says. “The uniqueness of this condition is that it is unfolding in real time, and there’s a lot of uncertainty. With a lot of chronic illnesses, we at least have a sense of the prognosis and the course of the illness, but long COVID is different for every single person.”
Although many of the patients who enter UT Health Austin’s Post-COVID-19 program have access to therapy outside the clinic, many practicing therapists lack a deep understanding of the lived reality of patients with long COVID. By participating in the therapy program, it allows patients to access mental health professionals who better understand what they’re going through both physically and mentally. Patients also have access to an art therapy group developed by Sam Bazzi, a graduate researcher at Dell Med. During this program, patients gather online once a week to participate in a therapy session centered on creating a piece of art that reflects some aspect of long COVID and shares their creation with other patients that have had similar experiences. For Carter, it was especially helpful to be in a group of people who understood each other’s challenges despite each experiencing a different range of long COVID symptoms. “Tears were shed and shared, but there was also laughter and appreciation,” Carter says. “We were all fighting to recover our health.”
Getting to the Bottom of Long COVID
The good news is that Brode says that most patients who have come through UT Health Austin’s Post-COVID-19 program have shown signs of recovery. While many of these patients may never be as healthy as they were prior to contracting COVID, even partial recovery can make a major difference in their quality of life. The bad news, however, is that researchers still have no conclusive evidence for what is causing long COVID, making it difficult to treat and predict who may develop it in the future. But while the origins of long COVID remain a mystery, Melamed and other researchers have found some titillating leads.
As part of UT Health Austin’s research program funded by the National Institutes of Health, Melamed worked with a consortium of researchers from several universities to study how COVID-19 affects the immune system. These researchers had noticed that many patients at UT Health Austin and other long COVID clinics around the country were producing antibodies in response to COVID infections that may have seeded autoimmune disorders that are responsible for their lingering systems. “The mystery with the auto-antibodies we’re discovering is that we don’t know if they are new post-COVID or if patients may have had autoimmune diseases prior to COVID, but just weren’t having any symptoms,” Melamed says.
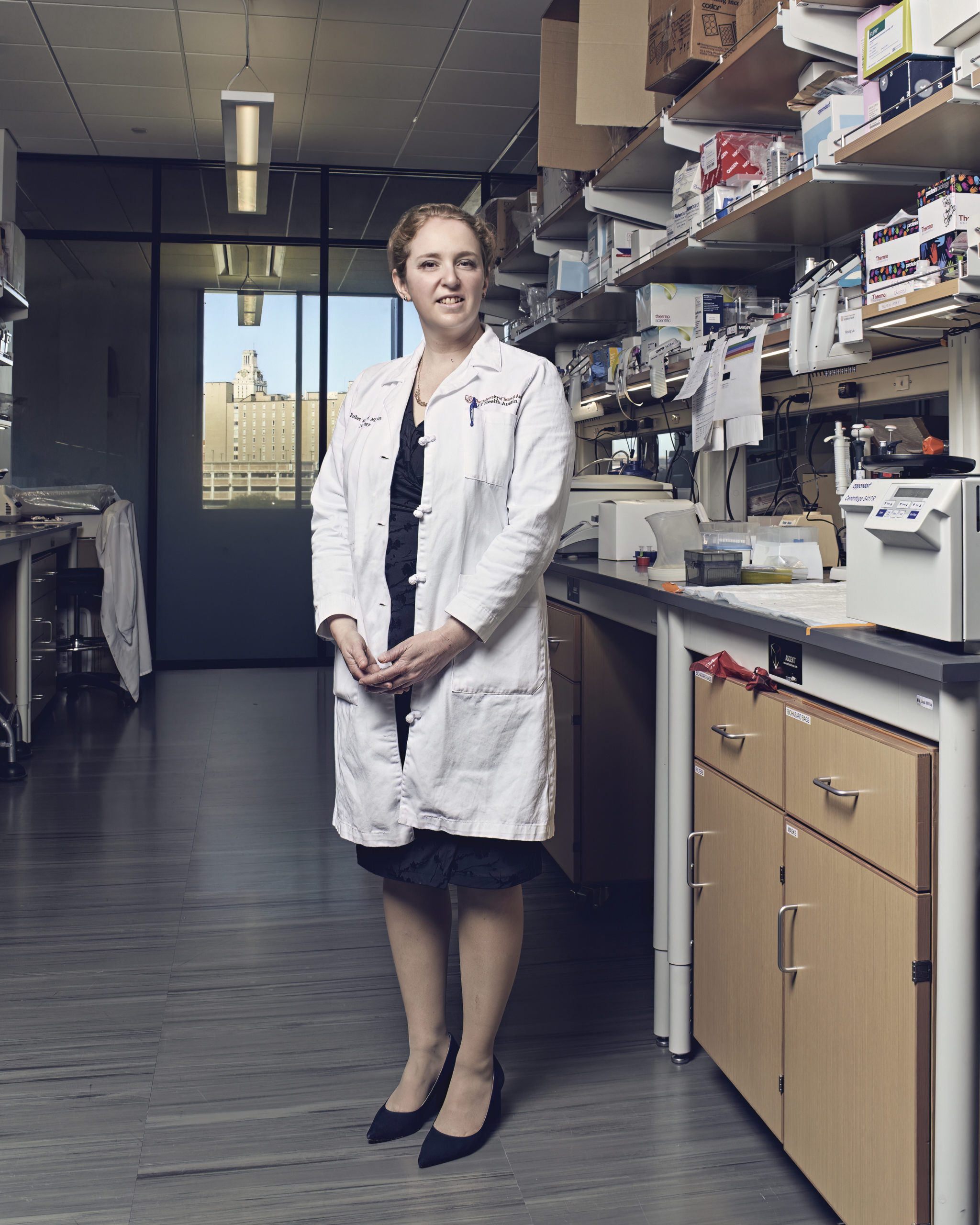
Another major question Melamed and her colleagues are exploring is how the body’s immune response to COVID impacts the brain. Many long COVID patients present have neurological symptoms such as difficulty concentrating or memory loss, which is similar to a condition known as “chemotherapy brain” that patients undergoing treatment for cancer experience. Shelli Kesler, a courtesy associate professor in Dell Medical School’s Department of Diagnostic Medicine, has found that the brains of long COVID patients do indeed resemble those of patients with chemo brain. Whereas in cancer patients the cause of these neurological symptoms can be traced to chemotherapy, it’s still unclear what causes these symptoms in long COVID patients. For example, says Melamed, it could potentially be the result of brain damage caused by viral inflammation or the COVID virus interrupting the flow of oxygen to the brain.
“Hopefully, we’ll start to get toward a better definition of what long COVID looks like neurologically,” Melamed says. “That should lead us towards identifying biomarkers in patients that can be followed to better understand outcomes in patients with neurological symptoms from COVID.”
The clinical and research components of UT Health Austin’s Post-COVID-19 program have played an important role in setting hundreds of long COVID patients on the path to recovery. After enrolling in the program and being put on an IVIG regiment, Carter’s health started improving for the first time in nearly a year and a half. While she is still not fully recovered and may never be able to compete at the same level in rowing before COVID, Carter has recently been able to start doing yoga again and has enrolled in a swim clinic to aid her recovery. She says it’s still difficult to face the reality of what she has lost to this illness, but she also is thankful for what she has regained through the physical and emotional support from the doctors at UT Health Austin.
“I think what they’re doing at Dell Med is really critical and necessary, and I am enormously grateful to all the dedicated researchers and clinicians at the clinic,” Carter says. “This kind of care needs to be made accessible for the thousands of people out there suffering with long COVID.”
Brode and Melamed are working on it. Based on caseloads of COVID-19 in and around Austin, Brode estimates that there are likely 30,000 Texans in the local area experiencing long COVID. Obviously, UT Health Austin’s Post-COVID-19 program can’t handle all these patients on its own, which makes community outreach essential. Most general physicians are already crunched for time and may only have a few minutes to meet with their patients in a clinic—far too little time to treat a disease as complex as long COVID. The result is that many general physicians pass their patients onto specialists who are often only looking at one side of a multi-faceted illness. This leads to a sense of frustration and hopelessness in many patients whose doctors are unable to point them to a path to recovery—or even effective symptom management.
The solution, Brode and Melamed say, is fostering strong relationships with clinicians in and around Austin, as well as the wider research community. As part of their work at UT Health Austin’s Post-COVID-19 program, Brode hosts workshops and seminars to provide the most up-to-date guidance and evidence to local doctors so that they can better help their own patients with long COVID. At the same time, Melamed is working with the National Institutes of Health and other universities to advance research on the causes of long COVID. By working together, they hope they will not only improve patient outcomes, but also shed some much-needed light on this mysterious illness.
“There’s a spirit of collaboration to meet the crisis of this long pandemic,” Brode says. “There are so many patients out there that we need all hands on deck so we can figure this out together.”
CREDITS: Illustration by Anna Godeassi; photographs by Matt Wright-Steel