One of the Last People to Live in an Iron Lung Is a Longhorn

Paul Alexander still remembers the sound of the screen door slamming on that rainy July day in 1952.
The then-6-year-old had just run inside after playing in the field behind his Dallas home. He was feverish and his neck ached. He walked in barefoot, dragging mud onto the kitchen floor. The door sprang shut behind him. He knew his mom would be mad when she saw the mess, but he was taken aback by the fear in her voice.
“God, please, no,” she said. She knew then polio had come for her son.
1952 was riddled with fear for many parents. It was the worst year for polio in the U.S., with nearly 60,000 cases reported across the country. Some cities shut down popular gathering places—movie theaters, swimming pools, bars, bowling alleys. The virus most commonly affects children, entering the body through the mouth via tiny particles of contaminated feces or, more rarely, droplets from a sneeze or cough. It can lead to flu-like symptoms and has the potential to invade a person’s spinal cord or brain, causing paralysis and potentially death.
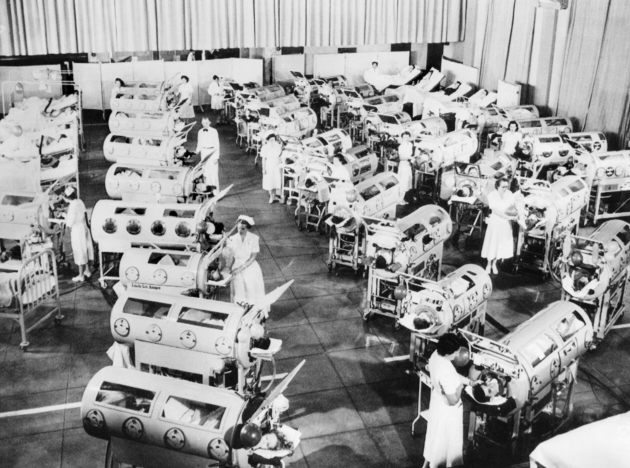
For Alexander, the infection started as body aches and a high fever, but not long after, he lost his ability to walk, swallow, and breathe. Doctors performed a tracheotomy and put him in an iron lung—a sealed tank used to treat polio patients who had trouble breathing on their own. During the epidemic, hospital wards were lined with these respirators. They stimulate breathing by varying air pressure to compress and depress the chest. Children typically spent a couple weeks in one while recovering from the disease, lying on their backs, unable to do much. But Alexander didn’t get out of his.
Eighteen months after he was admitted, doctors said he could go home, thinking he wouldn’t live much longer. His body was nearly completely paralyzed from the neck down, and he couldn’t breathe outside the iron lung. His family brought him—and the lung—home and had what they thought would be their last Christmas together.
But Alexander is still alive today. He’s 74 and resides in Dallas—and for the second time in his life, living through the outbreak of a virus that he is at a high risk of suffering from. Unlike the polio virus, the coronavirus hasn’t been disproportionately impacting children. Those most at risk of developing a severe case of COVID-19 are adults over 65 and those with underlying medical conditions. Alexander checks both boxes.
As the world awaits a vaccine, Alexander and his caretakers are limiting contact with others. He still relies on an iron lung to keep him alive. In fact, he’s one of the last people in the world still using the machine.
“It’s like a big tin can,” he tells me over Skype one morning in June. His head sticks out of the yellow tube, and I can hear the machinery expanding and compressing in the background. Between the noise and the fuzzy screen, it’s sometimes hard to make out what he’s saying. I find myself asking him to repeat himself. Alexander is patient with me and starts his sentences over. It’s not the most efficient way to conduct an interview, but we’re making do, given the circumstances.
Though more modern ventilators have been invented over the years, Alexander stuck with his iron lung. As a boy he learned how to breathe without it for extended periods of time—a skill that opened doors for him. When he was 8, a physical therapist taught him how to “frog breathe,” or use muscles in his mouth and throat to gulp air into his lungs.
Alexander was wary of health care professionals, scarred from the times in the hospital when they’d forced him to try to breathe outside the lung, causing him to pass out. But the therapist convinced him to keep trying by making a deal with him: if he could learn to breathe outside the lung for three minutes, she would give him one of her boxer puppies.
“It was difficult, but I worked at it,” Alexander says.
After working at it for a year, the puppy was his. Breathing on his own meant he could spend hours outside the iron lung. He adapted in other ways as well. His father fashioned a stick that he could put in his mouth to play with his toys. (Today, he uses a similar instrument to dial the phone and type on a keyboard.) He learned how to paint and write with a paintbrush or pencil in his mouth, too.
As he grew older, he realized that if he wanted to be successful at something, it would have to be something of the mind. “I had to go to school,” he says. “There was no other way.”
One of the first students to attend the homebound program in his school district, Alexander ended up graduating at the top of his class. He then attended Southern Methodist University before transferring to UT to study economics and finance. “I needed something bigger,” he says. For the first time in his life, he was away from home.
When he got to Austin, though, his hired caretaker never showed up. He refused to call his parents for help, fearing they’d take him home. “I was so determined to do this,” he says. “I thought, I’m going to die or I’m going to go to school.”

His first month at UT, students in his residence hall took care of him. They fed him and took him to class in his wheelchair. He says a lot of his professors were “angels” and believed in him. It took him seven years, but he graduated in 1978. And he wasn’t done with school yet. He attended UT Law, but this time around, the professors weren’t as encouraging. Alexander remembers one who brought him into his office and told him, “You don’t look like a lawyer,” and, “You’re not going to pass my class.” But he did.
He graduated in 1984 and passed the bar two years later. He spent decades as a lawyer in Dallas, practicing family law and taking on bankruptcy cases, representing clients in court from his wheelchair. When new clients came into his office, they’d see the iron lung and often ask, “What is that?”
It’s a moment Kathy Gaines, his caretaker of over 30 years, knows well. At the start of his career, he put an ad in the newspaper for a caretaker and Gaines responded. Before she met him, she’d never seen an iron lung before. “I walked in, and there was this big, yellow, monster machine, and I was like, ‘Woah, what the hell is this?’” she says. “Paul likes that—it’s like, ‘Wow, that’s a cool car,’ you know?”
She started taking on tasks: cooking his meals, shaving his beard, brushing his teeth, tying his tie—“You have to know how to tie a tie to help a lawyer,” she says—and eventually began working for him full time. Over the years, she’s learned everything about him. She can tell if he’s not getting enough oxygen, or when he’s dehydrated. “I know his body language so well, better than him,” she says. “He gets mad at me. I say, ‘Paul, drink.’ He says, ‘I’m not thirsty.’ I say, ‘Paul, you are thirsty, drink.’”
As Alexander aged, it became more difficult to breathe on his own. Now, he’s completely confined to his iron lung. He stopped practicing law in the last few years and set a new goal: telling his life’s story. Lying on his back in the iron lung, he wrote using a pen attached to a plastic stick. A mirror above his head reflected his notes back to him. He self-published his memoir, Three Minutes for a Dog, in April. It took eight years to complete. Gaines calls it “his big victory.”
One of the reasons Alexander wants to share his story is so people understand the severity of polio. After American virologist Jonas Salk developed a successful polio vaccine in 1955, countries began spearheading immunization campaigns. Since 1979, no cases of polio have originated in the U.S., meaning many Americans don’t understand how prevalent polio once was. Children in the U.S. are vaccinated against the disease by the time they’re 6. But vaccine-preventable diseases, like polio or measles or mumps, haven’t disappeared. Though it’s close to being eliminated, polio is still endemic in three countries: Afghanistan, Pakistan, and Nigeria. And “if we let ourselves become vulnerable by not vaccinating,” the Centers for Disease Control and Prevention warns, “a case that could touch off an outbreak of some disease that is currently under control is just a plane ride away.”
“Polio could come back,” Alexander tells me. Now that we’re living through a pandemic, his words, and the CDC’s, don’t sound alarmist at all. As I talk with Alexander, a living reminder of how an invisible virus can alter one’s life forever, it’s easy to draw parallels between the polio outbreak and the coronavirus pandemic. The calls to avoid gatherings of people. The fears. The anticipation of a cure. I find myself reading the pages of his memoir, in which he implores the world not to forget about the destructive consequences of polio, with a new sense of urgency. “It is extremely important,” he writes, “that you know what this is and what I have had to live with.”
From top: Courtesy of Paul Alexander; Alamy Stock Photo; courtesy of Paul Alexander